Introduction to Ethnic Skin Types
The United Kingdom is renowned for its multicultural society, with a population comprising a rich tapestry of ethnic backgrounds. This diversity brings with it a wide range of skin types, each exhibiting unique histological characteristics. From Fitzpatrick skin type I, common among those of Northern European descent, to type VI, more prevalent in individuals of African or Afro-Caribbean heritage, the variation in pigmentation, dermal structure, and response to environmental factors is significant. Recognising these differences is not merely an academic exercise; it is an essential aspect of clinical practice in dermatology and aesthetic medicine. Understanding the histological nuances between ethnic skin types underpins safe and effective laser treatments, helping clinicians avoid complications such as hyperpigmentation or scarring that disproportionately affect patients with higher melanin content. As the UK’s population continues to diversify, practitioners must be adept at tailoring their approach to meet the needs of all patients, ensuring equitable care and optimal outcomes.
2. Histological Characteristics of Ethnic Skin
The histological differences among ethnic skin types play a crucial role in determining their response to laser treatments. These differences are mainly observed in melanin content and distribution, stratum corneum thickness, and vascular architecture. A detailed understanding of these characteristics is essential for practitioners aiming to deliver safe and effective laser therapies across diverse populations.
Melanin Content and Distribution
Melanin is the primary pigment responsible for skin colour and provides photoprotection by absorbing ultraviolet (UV) radiation. The total amount of melanin, as well as its type (eumelanin versus pheomelanin), varies significantly among different ethnic groups. Individuals with darker skin types (Fitzpatrick IV–VI), commonly seen in African, South Asian, and Middle Eastern populations, have more abundant and larger melanosomes that are dispersed singly throughout the epidermis. Conversely, lighter skin types (Fitzpatrick I–III), prevalent in Northern European populations, contain smaller melanosomes that are often grouped within keratinocytes.
| Ethnic Group | Melanin Level | Melanosome Size | Distribution Pattern |
|---|---|---|---|
| African/Caribbean | High | Large | Singly dispersed |
| South Asian/Middle Eastern | Moderate–High | Medium–Large | Mainly singly dispersed |
| Northern European | Low | Small | Grouped within cells |
Stratum Corneum Thickness
The stratum corneum, the outermost layer of the epidermis, also exhibits variation between ethnicities. Studies indicate that individuals with African descent tend to have a thicker stratum corneum compared to those of European or East Asian descent. This increased thickness offers enhanced barrier protection but may also affect laser penetration and absorption, requiring adjustments in treatment parameters.
Comparative Thickness of Stratum Corneum by Ethnicity:
| Ethnic Group | Relative Thickness of Stratum Corneum |
|---|---|
| African/Caribbean | Thicker |
| Northern European | Moderate |
| East Asian | Thinner |
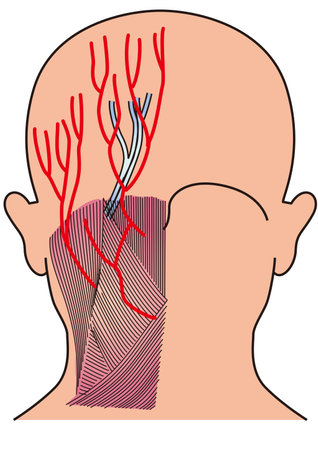
Vascular Differences in Ethnic Skin
The density and depth of dermal blood vessels can differ among ethnicities, influencing how energy from lasers interacts with the skin. For example, individuals with lighter skin types often have more visible superficial vasculature due to lower melanin masking effects, which can impact vascular-targeted laser procedures. In contrast, deeper or denser vessels in darker skin may necessitate modifications in wavelength or pulse duration to avoid complications such as hyperpigmentation or scarring.
Summary Table: Key Histological Features by Ethnic Group
| Feature | African/Caribbean | Northern European | East Asian |
|---|---|---|---|
| Melanin Content | High | Low–Moderate | Low–Moderate |
| Stratum Corneum Thickness | Thicker | Moderate | Thinner |
| Vascular Visibility* | Less visible** | More visible | Variable |
| *Influences laser parameter selection | |||
| **Due to higher melanin masking effect | |||
An in-depth appreciation of these histological distinctions enables clinicians to tailor laser treatments with greater precision, improving outcomes while minimising risks such as post-inflammatory hyperpigmentation or scarring in ethnically diverse patients.

3. Impact on Laser-Tissue Interaction
Histological differences among various ethnic skin types significantly influence the way skin interacts with laser energy, a core consideration for practitioners in the UK where patient populations are increasingly diverse. One of the main factors is melanin content and distribution within the epidermis and dermis. Higher melanin levels, as found in Fitzpatrick skin types IV to VI, result in increased absorption of laser light, particularly at shorter wavelengths. This increased absorption can heighten the risk of unwanted thermal injury, such as post-inflammatory hyperpigmentation or even burns, if inappropriate parameters are selected.
Additionally, the structural arrangement of collagen fibres and the density of blood vessels can differ among ethnic groups, altering how light is scattered and diffused within the tissue. For instance, a denser collagen matrix can increase scattering, reducing the penetration depth of certain laser wavelengths. In practical terms, this means that energy may be dissipated more superficially in some ethnic skins, which could compromise treatment efficacy for deeper targets such as hair follicles or vascular lesions.
The rate at which heat dissipates from targeted chromophores also varies depending on skin histology. Thicker epidermal layers and higher lipid content, more common in some darker phototypes, can modify thermal relaxation times. This necessitates careful adjustment of pulse duration and fluence during laser procedures to avoid collateral damage while achieving desired results. For clinicians working in the UK’s multicultural context, understanding these nuances is essential for optimising safety and outcomes during laser treatments.
4. Clinical Implications for Laser Treatment Planning
The diverse histological features of ethnic skin types have direct consequences on laser treatment strategies within the UK, where multicultural populations are increasingly seeking cosmetic and medical dermatological interventions. Clinicians must employ a comprehensive, individualised approach to patient assessment and laser parameter selection to ensure both efficacy and safety.
Patient Assessment: Understanding Ethnic Skin Variability
Initial consultation should include a detailed history and thorough examination of the patients skin type, using the Fitzpatrick scale as a baseline but expanding assessment to encompass subtler variations in pigmentation, dermal thickness, and propensity for post-inflammatory responses. It is essential to enquire about prior reactions to cosmetic procedures, family history of keloid formation, and current use of topical or systemic agents that may influence skin healing or pigmentary response.
Laser Parameter Selection: Customising for Safety and Effectiveness
Adapting laser settings to suit histological differences in ethnic skin is crucial to minimise adverse effects such as hyperpigmentation, hypopigmentation, or scarring. The table below provides a reference guide for selecting appropriate laser parameters based on common ethnic skin characteristics encountered in UK clinics:
| Ethnic Skin Characteristic | Recommended Laser Type | Wavelength (nm) | Pulse Duration | Fluence Adjustment |
|---|---|---|---|---|
| Darker Phototypes (IV-VI) | Nd:YAG (Long-pulsed) | 1064 | Longer pulse duration | Start low, titrate up cautiously |
| Tendency for Post-inflammatory Hyperpigmentation | Pulsed Dye Laser or Fractional Non-ablative | 585–595 / 1550–1927 | Shorter pulses for less thermal spread | Lower fluence, multiple sessions preferred |
| Keloid/Hypertrophic Scar Prone | Avoid aggressive ablative modalities; consider fractional lasers with conservative settings | – | – | – |
| Lighter Asian Skin (III-IV) | Alexandrite or Diode Lasers (with caution) | 755 / 800–810 | Moderate pulse duration | Cautious test patching recommended |
Risk Mitigation Strategies in Practice
Patch testing: Always conduct small-area test pulses before full treatment to evaluate skin reactivity and pigment changes over several weeks.
Cooling protocols: Employ dynamic cooling devices or chilled gels to protect the epidermis.
Treatment intervals: Allow extended intervals between sessions for sufficient healing and accurate assessment of pigmentary response.
Patient education: Discuss realistic outcomes, potential risks, and pre-/post-treatment care tailored to their specific skin type.
The UK Perspective: Emphasising Inclusivity and Best Practice Standards
The UK’s ethnically diverse population requires practitioners to remain vigilant regarding subtle variations within broad phototype categories. Adherence to evidence-based guidelines—alongside ongoing professional development in ethnic dermatology—ensures that all patients receive equitable, safe, and effective laser treatments tailored to their unique histological profiles.
5. Potential Complications and Management Strategies
Ethnic variations in skin histology contribute significantly to the types and frequencies of complications following laser treatments. Individuals with higher Fitzpatrick skin types—commonly seen in those of African, South Asian, Middle Eastern, and East Asian descent—are particularly prone to post-inflammatory hyperpigmentation (PIH), hypopigmentation, and keloid scarring. These adverse effects are less common but still possible in lighter skin phototypes. Understanding these complications is critical for practitioners across the UK, given the nation’s increasingly diverse population.
Common Laser-Related Side Effects
Among darker skin types, PIH is perhaps the most prevalent complication post-laser therapy. It manifests as darkened patches at the treatment site due to melanocyte hyperactivity triggered by inflammation. Hypopigmentation—loss of skin colour—may also occur, especially when aggressive settings or inappropriate wavelengths are used. Keloid formation and hypertrophic scars are other concerns, particularly in individuals with a known personal or family history of abnormal scarring. Erythema, blistering, and transient textural changes are universal risks but may resolve more slowly in richly pigmented skin.
Prevention Strategies
- Device Selection: Choose longer wavelength lasers such as Nd:YAG (1064 nm) for hair removal or vascular lesions in darker skin, as these penetrate deeper and reduce epidermal melanin absorption.
- Parameter Adjustment: Employ lower fluences and longer pulse durations to minimise thermal damage to the epidermis.
- Skin Preparation: Encourage pre-treatment use of broad-spectrum sunscreens and topical agents such as hydroquinone or azelaic acid to suppress melanocyte activity where appropriate.
Treatment of Complications
- PIH: Initiate early intervention with topical depigmenting agents (e.g., hydroquinone, retinoids) and strict photoprotection. Consider referral to dermatology for persistent cases.
- Keloids/Scars: Use silicone gel sheets, intralesional corticosteroids, or pressure therapy if keloids develop. Early identification is key to prevent progression.
- Erythema/Blistering: Apply soothing emollients and monitor closely; secondary infection risk should be minimised with proper wound care.
Practical Guidelines for UK Practitioners
A thorough consultation—including discussion of ethnic background, family history of pigmentation disorders or scarring, and previous response to cosmetic procedures—is essential. Patch testing on a discreet area is advisable before full treatment. Culturally sensitive communication regarding realistic outcomes and potential risks can help manage expectations and build trust within Britain’s multicultural patient base. Ongoing training in skin-of-colour management remains crucial for all clinicians offering laser therapies in the UK.
6. Conclusion and Future Directions in the UK Setting
In summary, understanding histological differences in ethnic skin is crucial for delivering safe and effective laser treatments within the UK’s diverse patient population. Recognising variations in melanin distribution, epidermal thickness, and inflammatory response guides practitioners in selecting appropriate laser modalities and settings. These considerations reduce the risk of complications such as hyperpigmentation or scarring, which disproportionately affect individuals with darker skin types commonly seen in British Black, Asian, and minority ethnic (BAME) communities.
Best practice in the UK now demands a nuanced approach: thorough pre-treatment assessment, patient education about potential risks and outcomes, and careful post-treatment follow-up. Clinicians are encouraged to keep abreast of evolving technologies—such as longer wavelength lasers and advanced cooling systems—that can improve safety profiles for all skin types. Additionally, collaborative research within the NHS and academic settings should prioritise data on underrepresented groups to build a robust evidence base tailored to British demographics.
Looking forward, further investment in clinical training, patient outreach, and ongoing research will help ensure that advances in laser technology benefit everyone equitably. As Britain continues to grow more diverse, the dermatological community must evolve its practices to reflect this reality—championing inclusivity, individualised care, and scientific rigour at every step.